Lean healthcare: Improving surgical process indicators through prioritization projects
Abstract
Purpose: Implementing process management methodology through Lean Management and Design Thinking provides a new way to manage surgical blocks, maximize efficiency and adapt to the high variability of demand. This article presents our experience of implementing a set of improvement actions within the surgical process in the context of Lean Healthcare Processes. The project involved a total of 900 healthcare professionals over a 3-year period (2017-2019) and has impacted over 38,000 surgical patients each year at the Vall d'Hebron University Hospital in Barcelona, Spain.
The purpose of this article is to present a set of improvement projects within the surgical process and show the indicators that monitor its evolution. These projects have been implemented successfully in a hospital with high surgical complexity and indicate how health care professionals and process engineers can work together as a team to improve healthcare resources.
Design/methodology/approach: To evaluate the effectiveness of the actions presented, we propose a series of standardized indicators showing how our findings increase the efficiency of the surgical process. We also indicate Lean projects that can reduce patient waiting times and increase capacity. Below is a management model for the surgical process that considers industrial production criteria such as resource planning, optimizing the use of operating rooms and professionals' time and generating the best surgery combinations.
Findings: Projects that have increased efficiency in the surgical block the most have been standardized and converted into a model of action. This is designed to adapt to any level of complexity within the hospital process. The set of improvement projects has been divided into 6 stages: Programming, Material logistics process, pre-surgical stage, intra-surgical stage, post-surgical stage and transversal projects; each affecting a different area of the general hospital (not only the surgical unit). Furthermore, a visual flow chart was designed using the results of the project.
Findings from the study have led to a 15% increase in surgical capacity without the need for new resources. The average hospital stay also dropped from 7.2 days to 4.1 days. The flow vision in the care process improves the experience of both patients and health care professionals, who see their participation as part of the whole health care process.
Research limitations/implications: the projects were mainly developed at the Vall d'Hebron University Hospital. Although several of these projects have been carried out in other hospitals in Spain by the same team of process engineers, results may be biased when the team provides support within its own process department, compared to when it supports the local team in another hospital temporarily.
Another important limitation is that it takes several months to implement and consolidate the improvement projects and demonstrate improved indicators in a sustainable way over time. This matrix of projects is more than a specific action, a cultural change with the entire surgical department.
Originality/value: This study sets out a proposed practical example of applying surgery management tools in the surgical process. Our proposal can offer hospital managers and surgical coordinators an orderly, streamlined project guide for overall surgical performance indicators.
The main results from developing the model include the degree of satisfaction shown by healthcare professionals and the determined commitment from the center’s management team to promote process management using Lean methodology. This commitment continued despite the challenges of shifting the organizational structure towards process management, which is a complex task requiring a period of adaptation and learning.
Healthcare management has always prioritized increasing surgical patient safety and satisfaction. Patient flows are increased and resources used more efficiency by shifting the focus to the patient and the processes gone through during their hospital stay. This improvement project provides us with the best example of Lean methodology implementation if reinvested in bettering healthcare. This in turn increases the value perceived by patients, which is the ultimate purpose of the process.
Keywords
Full Text:
PDFDOI: https://doi.org/10.3926/jiem.4628
This work is licensed under a Creative Commons Attribution 4.0 International License
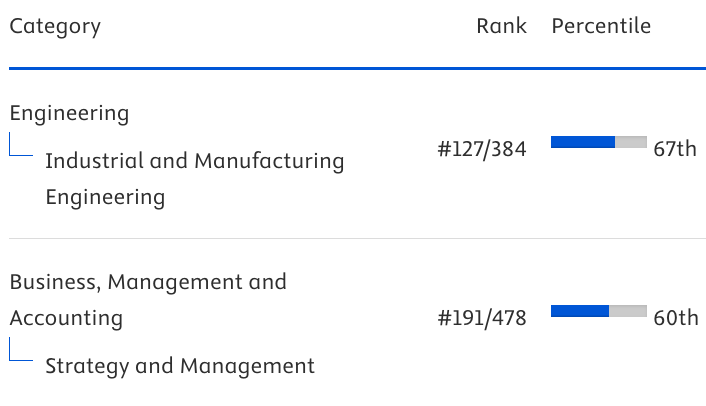
Journal of Industrial Engineering and Management, 2008-2025
Online ISSN: 2013-0953; Print ISSN: 2013-8423; Online DL: B-28744-2008
Publisher: OmniaScience